New paper provides roadmap for optimum maternal and fetal health
A new Briefing Paper, Diet in Pregnancy, published by the British Nutrition Foundation, combines the findings of academic research and recommendations from authoritative institutions, into a roadmap for good nutrition for parents and their babies, from preconception through pregnancy.
Diet in Pregnancy is published in the wake of the House of Lords Food, Diet and Obesity Committee’s report - Recipe for Health: a plan to fix our broken food system - which emphasises the importance of targeting pre-conception, pregnancy and early life to improve the overall health of people in the UK.
The British Nutrition Foundation paper, compiled by nutrition science experts and academics*, describes how a healthy, varied diet that meets the increased nutritional demands of pregnancy is essential to support fetal growth, development and maternal health, particularly as requirements for energy, protein and some micronutrients rise during this time.
However, data show that many women of childbearing age are not meeting recommended daily nutrient intakes, which can have a negative effect on their unborn baby’s development.
Sara Stanner, Science Director of the British Nutrition Foundation and co-author of the paper, said: “Dietary advice that encourages adequate intakes of the wide range of nutrients that contribute to maternal and fetal health, emphasising foods rich in folate, iodine, iron, calcium, vitamin D, is crucial. This should be accompanied by advice to take folic acid supplements pre-conception and during early pregnancy and to consider taking vitamin D supplements throughout pregnancy between the months of October to early March, or throughout the year for those considered at ‘high risk’.”
Pre-conception
The paper recommends that women considering a pregnancy should try to achieve a healthy bodyweight with a BMI of 18.5-25 preconception. There are no UK-specific guidelines for weight gain during pregnancy, but the NICE Guidelines on Maternal and Child Nutrition (NICE 2025) recommend that if people are interested in monitoring their weight change during pregnancy, they should be referred to the USA Institute of Medicine (IOM) (2009) guidelines for estimated healthy total weight change in singleton pregnancies.
Both overnutrition and undernutrition, before and during pregnancy, are associated with long-term negative consequences and can influence future risk of chronic disease, including type 2 diabetes and cardiovascular disease. Studies have shown that excess weight gained during pregnancy is associated with outcomes such as babies that are large for gestational age, and caesarean delivery, gestational diabetes mellitus, pre-eclampsia and postpartum weight retention for mothers. Conversely, inadequate gestational weight gain has been linked to low birth weight, small for gestational age and an increased risk of preterm birth.
Essential Fatty Acids
The paper states that omega 3 fatty acids found in foods such as oily fish are crucial for fetal cell membrane structure, new tissue formation, brain and retina development. Randomised controlled trials suggest modest benefits of long-chain n-3 polyunsaturated fatty acids, obtained through foods or via supplements, during pregnancy in extending gestation and increasing birth weight, alongside a potential reduction in preterm births and perinatal death risk.
Iron
34% of all women aged 19 - 65 years in the UK have low iron intakes, below the Lower Reference Nutrient intake**. Low iron status is linked to poor outcomes for both mother and baby, including premature birth and low birthweight. So, women of childbearing age should be advised to include iron-rich foods such as meat, eggs, fish, pulses, dark green leafy vegetables and fortified breads and cereals in their diet. Consuming foods rich in vitamin C is also important for people following a plant-based diet as vitamin C will help their body to absorb iron from plant foods.
Folate/folic acid
Taking a folic acid supplement before conception and during the first 12 weeks of pregnancy helps to prevent neural tube defects (NTDs), such as spina bifida, in babies. The latest NDNS data revealed that 83% of women aged 16 – 49 years had blood levels of folate that put them at increased risk of an NTD affected pregnancy. For the majority of women, a daily 400µg folic acid supplement is recommended, ideally from three months before pregnancy, to ensure levels are sufficient to support healthy development in early pregnancy. Where there is a greater risk of NTDs, maybe due to family history, a 5mg/day supplement may be recommended by a health care professional.
Iodine
Low iodine status during pregnancy can result in impaired infant neurological development and has been linked with reduced reading age and IQ in childhood.
The Scientific Advisory Committee on Nutrition has suggested that entering pregnancy with a good iodine status may be as important to a baby’s long-term health as consuming adequate iodine during pregnancy.
Latest figures1 show that average iodine status - measured using urinary iodine concentrations – is insufficient for girls aged 11 to 18 years and women of childbearing age (16 to 49 years). There has also been a significant decrease in iodine status over the last decade. Between 2013 to 2023, urinary iodine concentration decreased by 29% for girls aged 11 to 18 years and by 25% for adults aged 19 to 64 years.
Stanner said: “Milk and other dairy products are a main source of iodine for many people so, for those not consuming dairy products, it is important to get iodine from alternative sources such as eggs, fish, shellfish, and iodine fortified plant-based alternatives. Seaweed can also be a source of iodine but concentrations are variable and it is therefore not recommended to be eaten more than once a week during pregnancy.
“Although not advised routinely, supplements in the form of potassium iodide or potassium iodate may also be considered for people who may not be consuming sufficient iodine rich foods.”
Calcium and Vitamin D
Calcium is essential for the healthy development of a baby’s bones and teeth and vitamin D helps the body absorb calcium, so both are important from pre-conception throughout pregnancy; the latest NDNS data also shows that 17% of women aged 19 – 64 have low blood levels of vitamin D.
Stanner continued: “The advice for all women, including those who are planning a pregnancy, should be to consider taking a daily 10µg Vitamin D supplement in the autumn and winter months (October to early March), and consume foods that contain Vitamin D like eggs, oily fish, and fortified breakfast cereals. This is particularly important for women at higher risk of vitamin D deficiency, who should be advised to consider taking a supplement throughout pregnancy, including women with darker skin such as those of South Asian, African or African-Caribbean origin, or women who cover most of their skin when outside.”
Alcohol
Research shows that the only safe option is not to consume any alcohol at all from before conception throughout pregnancy.
During pregnancy
Stanner said: “To ensure that an unborn baby gets all the nutrients it needs for healthy development and growth from its mother, it is essential that women consume the right amounts of energy, protein, vitamins, and minerals during pregnancy and that they also avoid foods and drinks that can potentially be damaging to their unborn baby. In addition, women should be advised to limit the amount of caffeine they consume.
“While pregnant women should continue to consume enough iodine, folate/folic acid and vitamin D, and avoid drinking alcohol, research shows that iron and calcium are also particularly important at this time. It is not unusual for requirements for some women to increase with commonly low intakes of others.”
Caffeine
Pregnant women should be advised to not consume more than 200mg of caffeine each day – a mug of instant coffee typically has about 100mg caffeine and a mug of tea about 75mg. They should also be made aware that caffeine can be found in medicines such as cold and flu remedies, painkillers and stimulants, and in unexpected foods and drinks, including some herbal teas, hot chocolate, energy drinks, cola, milk and plain chocolate, as well as cold and flu remedies, painkillers and stimulants.
Training and resources
The Diet in Pregnancy paper also considers specific nutritional issues in teenage pregnancies and multiple pregnancies and references the barriers to uptake of the Healthy Start scheme, or similar, which provides prenatal vitamins and vouchers for nutrient dense foods for women who are living on low incomes. The paper highlights the need for appropriate training and resources for healthcare professionals to enable them to help women adopt healthier lifestyles and ensure better maternal and fetal health outcomes, potentially breaking cycles of poor health across generations.
For further information about diet in pregnancy and to download a handy guide for parents visit the British Nutrition Foundation’s website: [https://www.nutrition.org.uk/nutrition-for/pregnancy/]
Ends
*Dr Kathryn Hart, University of Surrey, Dr Alyson Hill, Ulster University; Dr Javier Gonzalez, University of Bath; Dr Anne de la Hunty, Editor Nutrition Bulletin; Prof Alison Gallagher, Ulster University; Sara Stanner, Science Director, British Nutrition Foundation
**the amount of a nutrient that is enough for only a small number of people in a group who have low requirements (2.5%)
The Briefing Paper can be accessed here: Diet in Pregnancy: A Review of Current Challenges and Recommendations. A British Nutrition Foundation Briefing Paper
1 National Diet and Nutrition Survey 2019 to 2023: report
For further information contact: Sophie Baillie at Sophie.baillie@consciouscomms.com or on 07766 707069.
Nourish to Flourish
Check out the infographic below for important nutrition and supplement information regarding pregnancy and the baby's development:
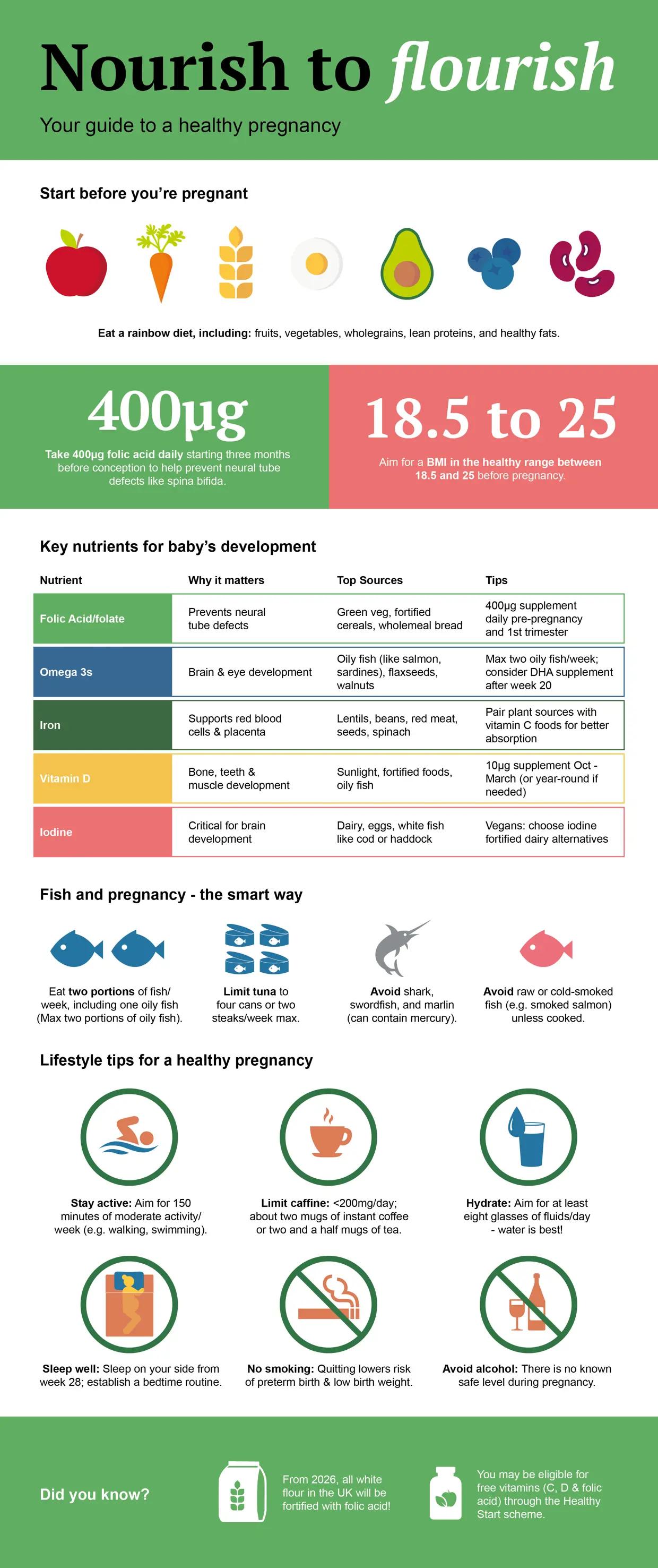
Download infographics
You can find a downloadable version of the infographic above, as well as further information about nutrients and pregnancy recommendations
Pregnancy Infographic Nutrients in Pregnancy Pregnancy Recommendations
About the British Nutrition Foundation
Connecting people, food and science for better nutrition and healthier lives
The British Nutrition Foundation is a charity that strives to prevent diet-related illness and promote health and wellbeing through evidence-based nutrition science. It provides a bridge between nutrition science, government, industry, healthcare, education and people, and is a conduit to a healthier, more sustainable food environment for all.
The British Nutrition Foundation’s team is made up of highly qualified and experienced nutrition scientists and educators who work to disseminate evidence-based peer reviewed research findings which: support industry strategy and healthy, sustainable product innovation; inform government policy and regulations; and help people build their knowledge, skills and confidence in making positive, food and lifestyle choices to help prevent illness and disease and promote health and wellbeing.
We safeguard our independence through robust governance, with an independent Board supported by an Advisory Committee and a Scientific Committee, both of which draw upon a broad range of experts from academia, government, industry, and public life. Our governance is weighted towards the scientific community, universities, and research institutes, and those from education, finance, media, communications, and HR backgrounds.
Funding for the British Nutrition Foundation is from membership subscriptions; donations; project grants from food producers and manufacturers, retailers and food service companies; conferences; publications, training, trusts, and foundations. The British Nutrition Foundation is not a lobbying organisation, nor does it endorse any products or engage in food advertising campaigns.
More details about the British Nutrition Foundation’s work, funding and governance can be found here.

Share this page
Article by British Nutrition Foundation